Earth Watch Report - Epidemic Hazards
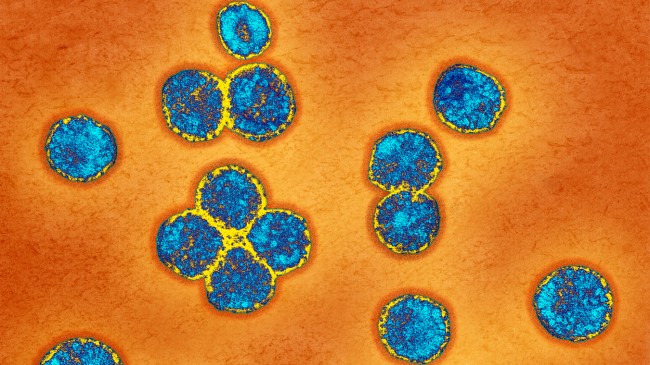
Image Source
***************************************************************************
| 17.06.2013 | Epidemic Hazard | Saudi Arabia | MultiProvinces, [Provinces of Eastern and Al-Qassim] |
Epidemic Hazard in Saudi Arabia on Thursday, 02 May, 2013 at 07:12 (07:12 AM) UTC.
Back| Updated: | Monday, 17 June, 2013 at 10:17 UTC |
| Description | |
| Saudi Arabia says four more people have died from a new respiratory virus related to SARS, bringing the total number of deaths to 32 in the kingdom at the center of the growing crisis. Overall, nearly 40 people have died from the virus since September, mostly in Europe and the Middle East. That’s according to local officials and the World Health Organization. The Saudi Health Ministry also said on Monday that it confirmed three more cases of the virus, including in a 2-year-old child. Officials are stillReport: Saudi MERS hospital outbreak had some SARS-like traits seeking clues on how easily it is spread between humans. The new virus is related to SARS, which killed some 800 people in a global epidemic in 2003, and belongs to a family of viruses that most often causes the common cold. | |
CIDRAP
Report: Saudi MERS hospital outbreak had some SARS-like traits
Jun
19, 2013 (CIDRAP News) – A study of the recent hospital outbreak of
MERS-CoV (Middle East respiratory syndrome coronavirus) in Saudi Arabia
reveals, among other things, that the virus spread in three hospitals
and that some patients transmit it much more than others do.
The report, published today in the New England Journal of Medicine,
shows that 21 of 23 cases involved person-to-person transmission in
healthcare facilities, and that 9 cases were in hemodialysis patients.
Testing
of more than 400 healthcare workers and household contacts of MERS
patients turned up only 7 additional cases, the report says, which
supports previous findings that the virus doesn’t spread very readily.
Investigators found that some patients didn't spread the virus to anyone
else, but one of them infected seven others.
The
report was prepared by a large international team with members from
Saudi Arabia, Canada, the United Kingdom, and the United States.
All
the hospitals involved are in Al-Hufuf (also spelled Al-Hofuf) in
Al-Ahsa governorate of eastern Saudi Arabia. The report covers 23
confirmed cases that were identified between from Apr 1 to May 23; 11
probable cases also are considered part of the outbreak.
As
of Jun 12, 15 of the 23 patients (65%) had died, 6 had recovered, and 2
remained hospitalized, the report says. Most of the patients were men,
and the median age was 56. Disease manifestations included fever in 20
patients, cough in 20, shortness of breath in 11, and gastrointestinal
symptoms in 8.
Most of the cases occurred at one
general hospital, called hospital A, which has 150 beds, plus a dialysis
unit. The event began on Apr 5 with admission of a patient with
dizziness and sweating, followed by a fever 3 days later. He was not
tested for MERS-CoV, but his son later had a confirmed case.
Another
patient, who was on dialysis, was admitted Apr 6 and put in a room next
to the first patient. By Apr 11 he had a fever, and he underwent
dialysis in the hospital on Apr 11 and 13. Between Apr 14 and 30,
MERS-Cov was confirmed in nine more patients who were receiving dialysis
in hospital A. Eight of these cases developed before or within 1 day
after infection control steps were taken in the dialysis unit.
One
dialysis patient who had a confirmed MERS-CoV infection was admitted to
a medical ward on Apr 21. In the following week, two other patients,
located two and three rooms away from the dialysis patient, fell ill
with the infection.
The virus spread to "hospital C"
when a patient who was infected at hospital A underwent dialysis at
hospital C while sick. Two other patients at the latter hospital
subsequently were infected.
In addition, eight
MERS-CoV patients were transferred to "hospital D," a regional referral
hospital. One of those patients passed the virus to two others at
hospital D, and another passed it to a physician there, the authors
concluded.
The team monitored 217 household contacts
of patients with confirmed cases. They found only five cases—three
confirmed and two probable—in adult relatives of three of the patients.
One of them was treated at another hospital, "hospital B," where the
report lists no other cases.
Only two confirmed cases
were detected among more than 200 healthcare workers who were monitored
after exposure, according to the report.
In mapping
transmission chains, the team found that one patient passed the
infection to seven other people, one passed it to three others, and four
transmitted it to two persons each. The authors say this variability in
transmission is "reminiscent of SARS" (severe acute respiratory
syndrome), which is caused by another coronavirus. Some patients in the
SARS epidemic in 2003 were described as "super spreaders."
The
median incubation period in the outbreak was 5.2 days (95% confidence
interval, 1.9 to 14.7 days). On the basis of recent MERS cases, the
World Health Organization has said the incubation time may run as long
as 10 to 14 days.
The investigators obtained full
genome sequences from isolates from four patients. From a phylogenetic
analysis of these sequences and from other data, they estimated that the
date of the most recent common ancestor of MERS-CoV was Aug 18, 2011.
This broadly agrees with the conclusion of a German team that, in a Lancet Infectious Diseases report this week, estimated the date of the most recent common ancestor as mid-2011.
The
authors were unable to determine if the hospital outbreak involved just
one, or more than one, transmission of the virus from the community.
Also,
they couldn't answer another key question about the virus: whether
person-to-person transmission occurred through respiratory droplets or
direct or indirect contact and whether aerosol transmission occurred
over a distance of more than 1 meter.
The report says
the pattern of the outbreak is consistent with the assumption that
patients were infectious only when they had symptoms, but this doesn't
rule out transmission during the incubation period or during
asymptomatic infection.
In other findings, the
authors note that the survival rate was higher for patients who were
identified through active surveillance than for those who were
identified clinically. They say the likely reason was that active
surveillance was better at picking up less-severe disease.
Assiri A, McGeer A, Perl RM, et al. Hospital outbreak of Middle East respiratory syndrome coronavirus. N Engl J Med 2013 (Early online publication). [Abstract]
******************************************************************************
CDC expert reports some anomalies in Jordan MERS cases
Jun 19, 2013 (CIDRAP News) – Eight Jordanians who had MERS-CoV
(Middle East respiratory syndrome coronavirus) infections in a hospital
outbreak more than a year ago, as determined by recent blood tests,
didn't quite match the profile of more recent cases, according to a CDC
expert.
Most of the eight people did not have preexisting diseases, and
one of them had no symptoms, said Mark Pallansch, PhD, director of the
CDC's Division of Viral Diseases.
The majority of MERS-CoV cases reported in recent months involved
patients who had preexisting health problems such as diabetes or heart
disease. And the asymptomatic case appears to be the first one reported.
The eight cases were associated with a hospital outbreak in Zarqa,
Jordan, in April 2012. The cause of the outbreak was a mystery at the
time, because MERS-CoV was not discovered until June of last year, when a
Saudi man died of his infection.
The Jordan outbreak involved 11 cases, 2 of them fatal. Samples
from the patients were stored, and later analysis led to confirmation of
the virus in the two fatal cases. The WHO said the other cases probably
were MERS, but that couldn't be confirmed.
Earlier this week a Canadian Press report revealed that serologic
(antibody) tests of 124 people related to the Jordan cluster had turned
up 8 more cases, raising the number of confirmed cases in the outbreak
to 10. The testing was done by the CDC in collaboration with Jordanian
health officials.
Pallansch provided more details on the study in an interview. He
cautioned that the findings are preliminary, because the CDC has had few
serum samples from MERS-CoV patients with which to validate the two new
serologic tests that were used.
"There's always a caveat that we could have subsequent testing change some of the results," he said.
Six of the eight cases were in healthcare workers and were part of the hospital illness cluster, Pallansch said.
One of the other two, the asymptomatic case, was in a household contact of one of the
confirmed cases, he reported. The other one involved a healthcare worker
who worked at the same hospital as the others. That person "by recall
did have an illness, but was not considered part of the cluster at the
time," he said.
Among the other six case-patients, "there was a range of illness,
but all were hospitalized, so it was reasonably severe," Pallansch said.
He said he is not aware of any other asymptomatic MERS-CoV cases.
Such cases are considered important because they suggest that people who
aren't sick can unknowingly spread the virus. Asymptomatic cases are
likely to be discovered only through serologic tests, which for MERS-CoV
have become available only recently.
Pallansch said he couldn't give any information about how the
first case-patient in the Jordanian cluster might have caught the virus
or about the patients' possible animal exposures. Officials are still
working on their report, he explained.
"This is a report that will go back to the Jordanian Ministry of
Health, and they'll make decisions about how it will be disseminated or
published," he said.
See also:
Related Jun 17 CIDRAP News story
Nov 30, 2012, CIDRAP News story
Bloomberg Business Week
AP News
New MERS virus spreads easily, deadlier than SARS
June 19, 2013
LONDON (AP) — A mysterious new respiratory virus that
originated in the Middle East spreads easily between people and appears
more deadly than SARS, doctors reported Wednesday after investigating
the biggest outbreak in Saudi Arabia.
More than 60 cases of what
is now called MERS, including 38 deaths, have been recorded by the World
Health Organization in the past year, mostly in Saudi Arabia. So far,
illnesses haven't spread as quickly as SARS did in 2003, ultimately
triggering a global outbreak that killed about 800 people.An international team of doctors who investigated nearly two dozen cases in eastern Saudi Arabia found the new coronavirus has some striking similarities to SARS. Unlike SARS, though, scientists remain baffled as to the source of MERS.
In a worrying finding, the team said MERS (Middle East respiratory syndrome) not only spreads easily between people, but within hospitals. That was also the case with SARS, a distant relative of the new virus.
"To me, this felt a lot like SARS did," said Dr. Trish Perl, a senior hospital epidemiologist at Johns Hopkins Medicine, who was part of the team. Their report was published online Wednesday in the New England Journal of Medicine.
Perl said they couldn't nail down how it was spread in every case — through droplets from sneezing or coughing, or a more indirect route. Some of the hospital patients weren't close to the infected person, but somehow picked up the virus.
"In the right circumstances, the spread could be explosive," said Perl, while emphasizing that the team only had a snapshot of one MERS cluster in Saudi Arabia.
Cases have continued to trickle in, and there appears to be an ongoing outbreak in Saudi Arabia. MERS cases have also been reported in Jordan, Qatar, the United Arab Emirates, Britain, France, Germany, Italy and Tunisia. Most have had a direct connection to the Middle East region.
In the Saudi cluster that was investigated, certain patients infected many more people than would be expected, Perl said. One patient who was receiving dialysis treatment spread MERS to seven others, including fellow dialysis patients at the same hospital. During SARS, such patients were known as "superspreaders" and effectively seeded outbreaks in numerous countries.
Perl and colleagues also concluded that symptoms of both diseases are similar, with an initial fever and cough that may last for a few days before pneumonia develops.
But MERS appears far more lethal. Compared to SARS' 8 percent death rate, the fatality rate for MERS in the Saudi outbreak was about 65 percent, though the experts could be missing mild cases that might skew the figures.
While SARS was traced to bats before jumping to humans via civet cats, the source of the MERS virus remains a mystery. It is most closely related to a bat virus though some experts suspect people may be getting sick from animals like camels or goats. Another hypothesis is that infected bats may be contaminating foods like dates, commonly harvested and eaten in Saudi Arabia.
Read More Here
Related articles
- Epidemic Hazard - Saudi Arabia, Eastern Province, Al-hasa : UPDATE (familysurvivalprotocol.com)
- News in Brief: On the trail of a new virus (sciencenews.org)
- New MERS virus spreads easily, deadlier than SARS (kfwbam.com)
- New coronavirus MERS, similar to SARS, but deadlier (voxxi.com)
- New MERS virus spreads easily, deadlier than SARS (courierpress.com)
- First Detailed Clinical Study Of Novel Coronavirus Cases In France Suggests That Incubation Period May Be Longer Than Previously Thought (medicalnewstoday.com)
- Saudis investigating possible second hospital outbreak of MERS coronavirus cases (vancouversun.com)
- Epidemic Hazard - Saudi Arabia, Eastern Province, Al-hasa : Two more people have died from novel coronavirus, a new strain of the virus similar to the one that caused SARS (familysurvivalprotocol.com)
- Study Reveals How New Respiratory Virus Spreads (news.health.com)
- Toronto SARS expert to go to Saudi Arabia to help with coronavirus (ctvnews.ca)

 News Editor
News Editor
No comments:
Post a Comment
Hello and thank you for visiting my blog. Please share your thoughts and leave a comment :)